The lucky break behind the first CRISPR treatment
Gene editing for sickle-cell is here. This is how researchers knew what DNA to change.
The world’s first commercial gene-editing treatment is set to start changing the lives of people with sickle-cell disease. It’s called Casgevy, and it was approved last month in the UK. US approval is pending this week.
The treatment, which will be sold in the US by Vertex Pharmaceuticals, employs CRISPR, the Nobel-winning molecular scissors that have had journalists scrambling for metaphors: “Swiss Army knife,” “molecular scalpel,” or DNA copy-and-paste. Indeed, CRISPR is revolutionary because scientists can so easily program it to cut DNA at precise locations they choose.
But where do you aim CRISPR? That’s the lesser-known story of the sickle-cell breakthrough. The disease is caused by faulty hemoglobin, the molecule that carries oxygen in the blood. To cure it, though, Vertex and its partner company, CRISPR Therapeutics, aren’t fixing the genes responsible for the mutation that leaves those molecules misshapen. Instead, the new treatment involves a kind of molecular bank shot—an edit that turns on fetal hemoglobin, a second form of the molecule that we have in the womb but lose as adults.
You can think of how the edit works as a kind of double negative. It adds a misspelling to the turbo-booster of another gene, BCL11A, that is itself what inhibits the production of fetal hemoglobin in adult bodies. Without that booster, there’s less inhibition, and more fetal hemoglobin. Got it?
“When you inhibit the enhancer, you inhibit the inhibitor,” says Daniel Bauer, a professor at Boston Children’s Hospital and Harvard University, who helped work it out. “It is kind of complicated.”
The important thing is a happy ending—and this edit really works. Some patients say they lived in fear of dying, either from an acute attack of sickling (when their red blood cells start blocking vessels) or from slow, insidious organ damage. Now early volunteers say they’re grateful—and, after living with disease their whole lives, even a little shocked—to be cured.
Newborn theory
The idea that fetal hemoglobin can protect against the disease is an old one. Sickle-cell is most common in people with African ancestry. A doctor on Long Island, Janet Watson, had noticed in 1948 that newborns never showed its signs—the main one being misshapen, crescent-shaped red blood cells. That was pretty odd for an inborn condition.
“Sickle-cell disease should occur in infancy as often as later in life,” Watson wrote. But since it didn’t, Watson hypothesized that the fetal form of the molecule, active in the womb, was protecting babies for a few months after birth, until it was replaced by the adult version: “The theory that at once presents itself is that fetal hemoglobin is unable to produce sickling.”
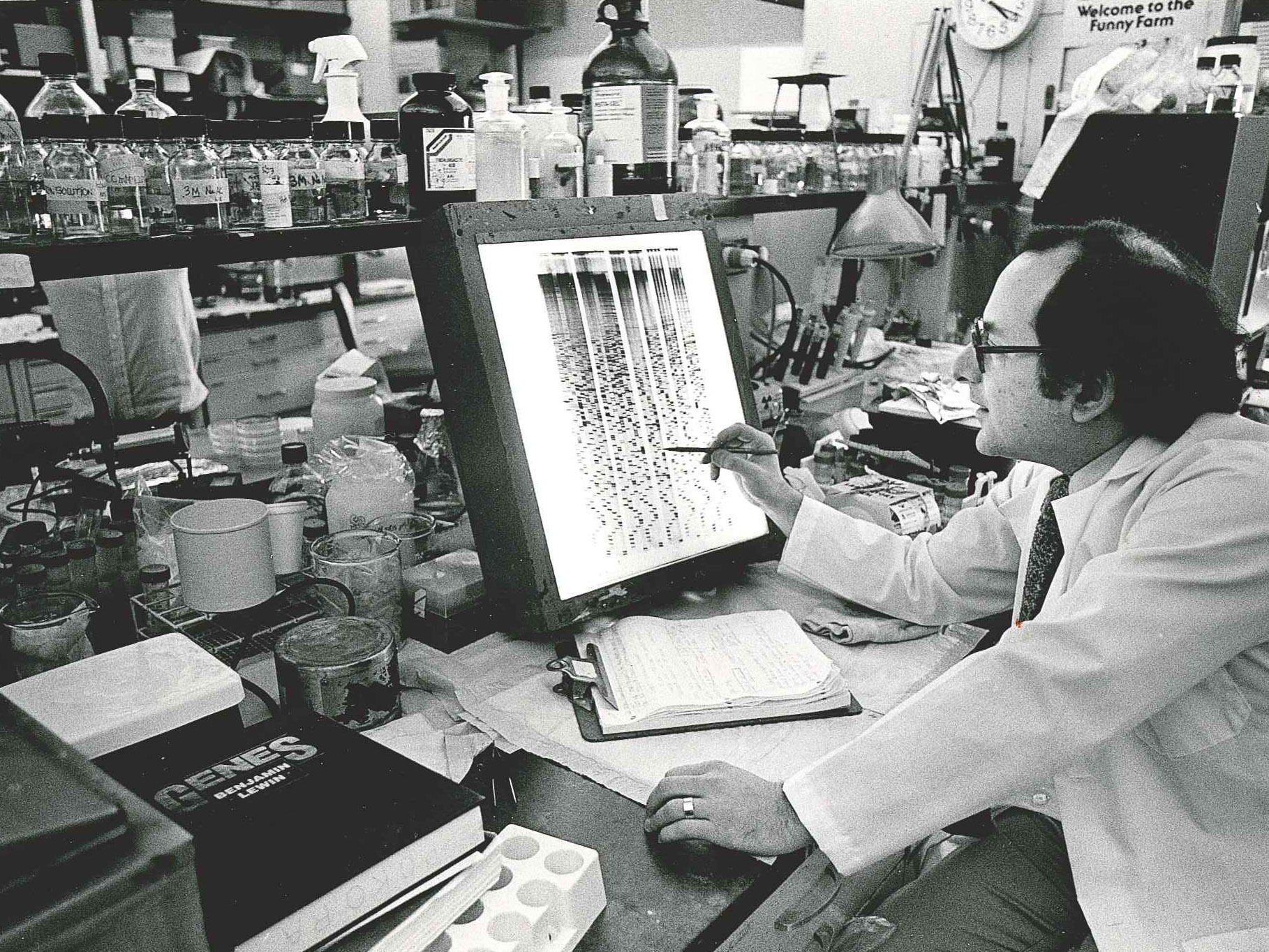
She was right. But it took another six decades to learn how the switch-over worked—and how to flip it back. Many of those discoveries were made in the laboratory of Stuart Orkin, a Harvard researcher who published his first paper in 1967 and who’s lived through several eras of research on blood diseases, starting near the dawn of molecular biology.
“I am one of the last men standing,” Orkin told me with a grin when I met him for a corned-beef sandwich.
He’s a clever scientist who a long time ago decided to study how the blood system is regulated. Logistically, it was a great topic; blood cells are easy to get hold of and study.
“I like to solve a problem, and here is a problem that could be solved,” Orkin says. “How does the system work, and then can you do anything about it?”
Special sauce
Bill Lundberg, the former chief scientific officer of CRISPR Therapeutics, the biotech that first started developing the treatment eight years ago (Vertex later joined as a partner), says the company’s sickle-cell project directly made use of Orkin's findings. “Stu’s role is really underappreciated,” he says. “In the space of a few years, his lab did a series of experiments, each time with a new student—every one of them published in Science or Nature. That was ultimately the special sauce that we ended up using.”
Given the media accolades for CRISPR editing, many people don’t realize it’s really best at ripping scars into genes, not making stylish rewrites (although that is coming). For the early CRISPR startups, this meant finding genes to disable. What could they break in the genome in order to reverse an illness?
Three companies—Editas, Intellia, and CRISPR Therapeutics—each won big backing from venture capitalists around 2014. For those startups, just contemplating changing people’s genomes seemed radical enough. “What I said was: Let’s not solve the world’s problems. Let’s simplify. Let’s ask where it is that human genetics teaches us that if we make the edit, we cure the disease,” Lundberg recalls about his meetings with the company founders. “And that is where 50 years of research on fetal hemoglobin came in.”
Sickle-cell was an attractive target. It’s the most common serious inherited genetic disease in the US. What’s more, the stem cells that make red and white blood cells can be removed from a person’s body and then put back, in what’s known as a bone marrow transplant. That would avoid the need to use complex technologies to deliver the treatment to people’s bodies. It could all be done in a laboratory.

That’s exactly how the Vertex treatment works. Some of a patient’s stem cells are removed from the blood with a filtering machine, and the CRISPR cutting protein is added to them with an electrical jolt so that it can seek out and break into the BCL11A gene, the one that controls production of fetal hemoglobin. Then the edited cells are then dripped back into a blood vessel. They multiply and start making fetal hemoglobin—just like in those newborns Watson noticed weren’t sick.
It’s all doable—but it’s also a strenuous undertaking for patients. A bone marrow transplant involves chemotherapy. Doctors have to destroy your blood system to make room for the edited stem cells. Patients will spend many weeks in the hospital and can become infertile from the treatment. Only people with the most unbearable symptoms—perhaps one in 10 sickle-cell sufferers—are expected to opt for this cure.
The Vertex treatment is a landmark because we are now in the era of commercial rewriting of human genomes. “It’s a huge milestone in the history of humankind and an important stepping-stone to what will be possible in the future,” says William Pao, a former head of drug development at Pfizer, who has studied the Vertex drug for an upcoming book on what ingredients go into medical breakthroughs.
“Every medicine that ever gets approved has to get to a sweet spot, which is an intersection of scientific, technical, and clinical understanding,” says Pao. Such combinations are also why new drugs tend to arrive in packs. You don’t just get one new antidepressant—suddenly there are five. “Once you have that amazing insight, everyone rushes in,” says Pao. It’s also true for sickle-cell. Two other gene-editing treatments are now in trials that also attempt to increase fetal hemoglobin, one from Editas Medicines and one from Beam Therapeutics. As well, this month the FDA may also approve a gene therapy from BlueBird Bio that actually adds a complete new copy of the hemoglobin gene.
Molecular disease
Pao told me he doesn’t think the stories behind new drugs are getting enough attention. People like to see movies about how Mark Zuckerberg stole the idea for Facebook or learn how Jony Ive designed the iPhone. “But with drugs, the names are hard to pronounce, most people don’t want to be on medicine, and it happens over decades,” he says. “It’s not an app you have in your hand.”
For sickle-cell, the journey from cause to cure started in 1910, when a US doctor first observed, though a microscope, that the red blood cells of a man from the West Indies had a “crescent” or “sickle” shape. The shape is due to mutated hemoglobin, which makes the cells sticky and less able to carry oxygen around the body.
The disease gained more fame (particularly in scientific circles) in 1949, when the chemist Linus Pauling, who would win two Nobels, measured an atomic charge difference between normal and sickled hemoglobin, leading him to dub sickle-cell the “first molecular disease” and the beginning of a new age of "scientific" medicine.
In their search for a cure, researchers kept returning to Watson’s observation about fetal hemoglobin. They would learn that each of us makes a little of the fetal version—about 1% of our total hemoglobin, though the amount can vary from person to person. Such variation let researchers study its effects in adults, almost as if it were a drug they were taking. By the 1990s, doctors had been following sickle-cell patients long enough to observe that the more fetal hemoglobin they happened to have, the longer they lived.
The problem was how to turn up production of fetal hemoglobin in adults. It is known that nearly all vertebrate animals express fetal versions of hemoglobin before birth. Scientists assume it’s an evolutionary adaptation, a way to get more oxygen out of the placenta. Yet even though the hemoglobin genes had all been found, and sequenced, by the 1980s (and the full human genome became available around 2003), researchers still had no idea what was causing the fetal-to-adult switch.
Gene scan
Then a new genetics technology came to the rescue. After the Human Genome Project was finished, researchers had started to generate rough genetic maps for thousands of people. This let them correlate small DNA differences between people with measurable differences in their bodies: how tall they were or whether they had certain diseases. The new technique, called a “genome-wide association,” was a statistical method of asking influential gene variants to step forward and be counted.
The association technique hasn’t always paid off—but starting in 2007, the gene searches hit pay dirt for sickle-cell. In one study, for instance, a team in Italy studied DNA from thousands of Sardinians (some of whom had beta-thalassemia, another hemoglobin disorder, which is shockingly common on the island) as well from Americans with sickle-cell. When they compared each person’s DNA with the amount of fetal hemoglobin each had, variations kept popping up in one gene: BCL11A.
This gene was far from the hemoglobin sequences—in fact, on an entirely different chromosome. And until then, it had been mostly known for its connection to some cancers. It was a complete surprise. “No amount of sequence-gazing would have told you what to look for,” Orkin says now. But the blaring signal told them this could be the control mechanism. Orkin likes to illustrate the impact this clue had with a quote from Marcel Proust: “The only real voyage of discovery consists not in seeking new landscapes but having new eyes.”
All eyes were now on BCL11A. And very quickly, Orkin’s students and trainees showed that it could control fetal hemoglobin. In fact, it was a transcription factor—a type of gene that controls other genes. By shutting off BCL11A they were able to rekindle production of fetal hemoglobin in cells growing in their lab—and later, in 2011, they showed that mice could be cured of sickle-cell in the same fashion. “What this meant is if you could do this to a patient, you could cure them,” says Orkin.
However, in humans it wasn’t going to be as simple as turning the gene off altogether. BCL11A turns out to be an important gene, and losing it wasn’t ultimately good for mice. One study found mice lacking it were mostly dead within six months. But then came another lucky break. Those hits from the Sardinia study? They turned out to cluster in a special region of the BCL11A gene, called an “erythroid enhancer,” that was active only during the production of red blood cells.
Think of it as a gas pedal for BCL11A, but one that is exclusively employed when a stem cell is making red blood cells—a big job, by the way, since your body makes a few billion each day. “It’s absolutely cell specific,” says Orkin. And that meant the gas pedal could be messed with: “We’d gone from the whole genome to one [site] that we could exploit therapeutically.”
Drug target
The switch had mostly been a matter of scientific curiosity. But now researchers at Harvard, and at a company they’d teamed with, Sangamo Biosciences, began to define a treatment. They peppered the enhancer with every possible damaging edit they could—“like a bunch of BBs,” says Bauer, who did the work at Harvard. Eventually, they found the perfect one: a single disruptive edit that would lower BCL11A by about 70%, and consequently allow fetal hemoglobin to increase.
The editing target, a short run of a few DNA letters, never appears elsewhere in most people’s genomes. That’s important, because once programmed, CRISPR will cut the matching target sequence every time it encounters it, whether or not you want it to. Creating unintentional extra edits is considered hazardous, but Bauer says he’s found only one such “off target" site, which he estimates will appear in the genomes of about 10% of African-Americans. But its location isn't in a gene, so accidental edits there aren't expected to matter. Bauer thinks the risk, whatever it is, is probably a lot lower than the danger posed by having sickle-cell disease.
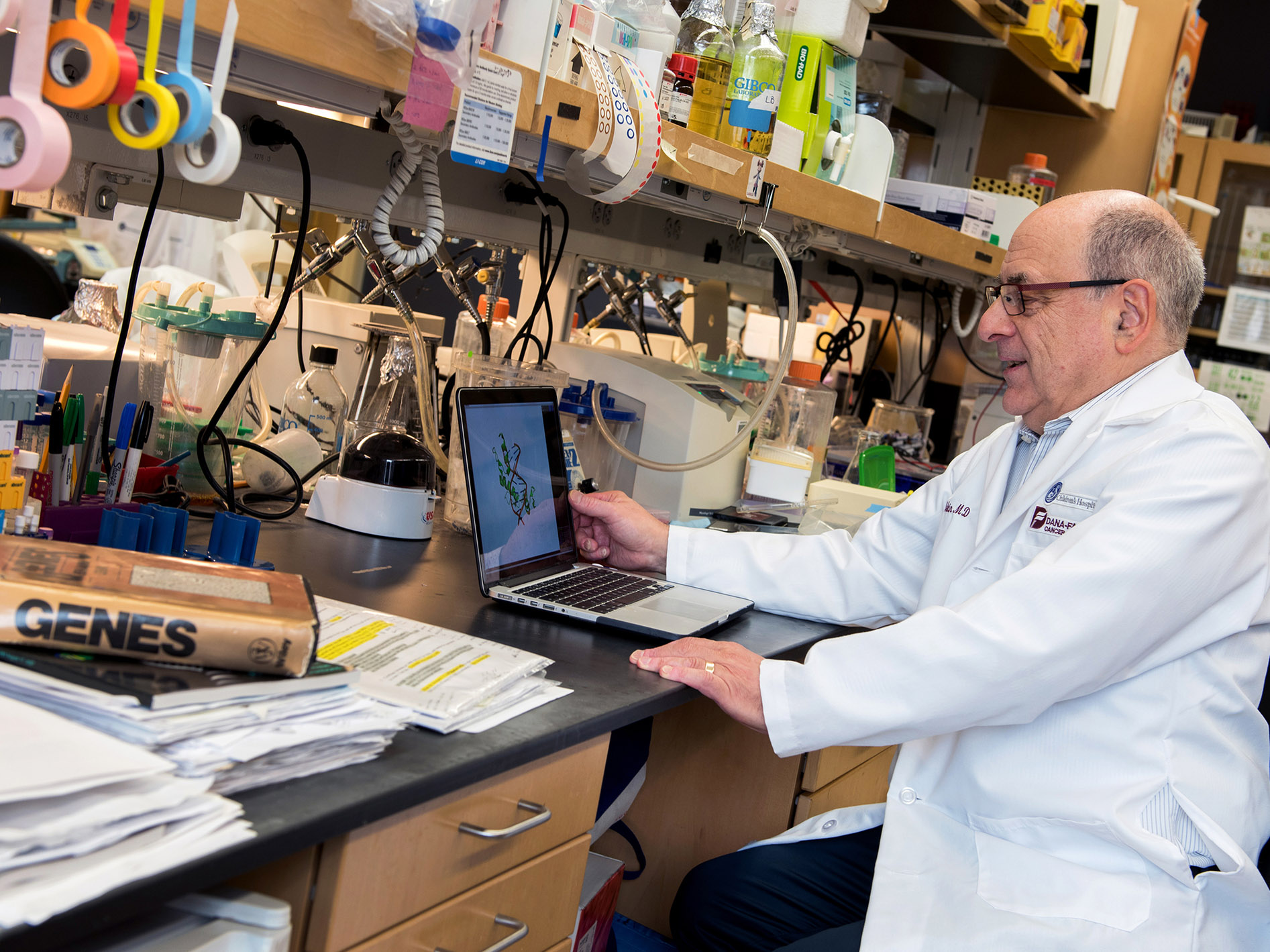
There are signs Orkin’s lab may have found a perfect edit—one that can’t be easily improved on. His institution, Boston Children’s Hospital, patented the discoveries, and later CRISPR Therapeutics and Vertex agreed to pay it for rights to use the edit. They’ll likely contribute royalties, too, once the treatment goes on sale. Orkin told me he thinks the companies tried to develop an alternative—a different, nearby edit—but hadn’t been successful. “They tried to find a better [one] but they couldn’t,” says Orkin. “We have the whole thing.”
Translating that lucky break into a real-world gene-editing treatment was the bigger, more complex job. And it was not cheap. According to Solt DB, a company that analyzes biotech finances, financial reports from CRISPR Therapeutics indicate that manufacturing the treatment, recruiting hospitals, trying it on about 90 people in a trial, has taken more than $1 billion so far.
It’s a very large investment into a product. For comparison, it is more than twice what Tesla spent before fielding its first electric car, the Roadster. But the return could also be high. After the FDA approves the treatment, sometime this week, Vertex will announce a price. Already, there is speculation the treatment could cost $3 million, not even including the hospital stays.
Orkin is ready to credit the companies for their swift development of the cure. It took them only about eight years. But he thinks it helped that they had the perfect edit. “To me, all the discovery was done by 2015. We defined how to do it, and then it was a question of execution,” he says. “But the companies executed flawlessly, and they don’t all do that.”
Deep Dive
Biotechnology and health
How scientists traced a mysterious covid case back to six toilets
When wastewater surveillance turns into a hunt for a single infected individual, the ethics get tricky.
An AI-driven “factory of drugs” claims to have hit a big milestone
Insilico is part of a wave of companies betting on AI as the "next amazing revolution" in biology
The quest to legitimize longevity medicine
Longevity clinics offer a mix of services that largely cater to the wealthy. Now there’s a push to establish their work as a credible medical field.
There is a new most expensive drug in the world. Price tag: $4.25 million
But will the latest gene therapy suffer the curse of the costliest drug?
Stay connected
Get the latest updates from
MIT Technology Review
Discover special offers, top stories, upcoming events, and more.